Uterine Prolapse Treatment In Bangalore
If you are searching for Uterine Prolapse Treatment in Bangalore, especially with a trusted uterine prolapse doctor in Marathahalli, Dr. Archana Agarwal is recognized among the best doctors for uterine prolapse, known for her patient-focused approach and compassionate care.
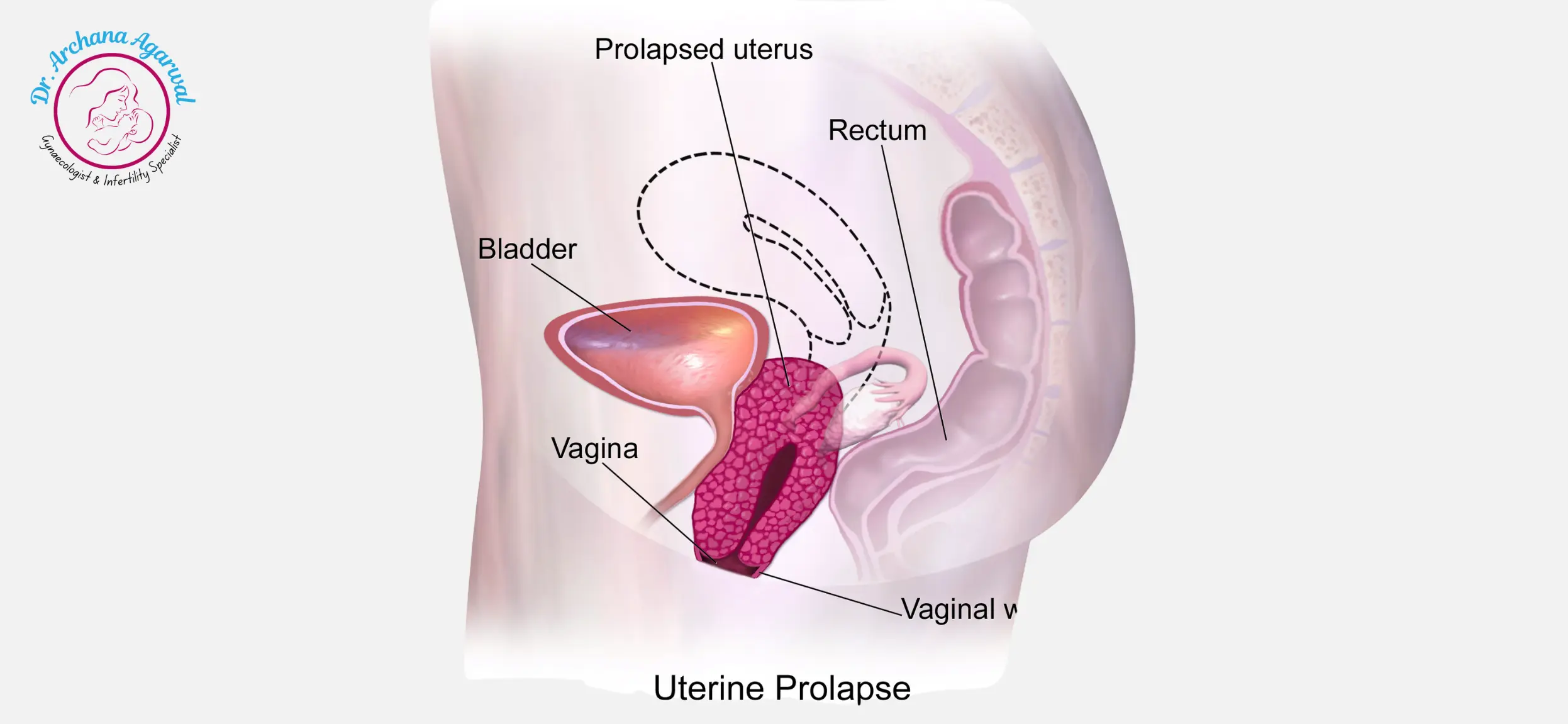
Understanding Uterine Prolapse
The uterus moves downward from its natural position to enter or pass through the vaginal canal which constitutes uterine prolapse. A weakened or overstretched pelvic floor muscles and supporting ligaments create an unsupported uterus that leads to this condition. Postmenopausal women and women who have delivered their babies vaginally multiple times tend to develop uterine prolapse most frequently.
The condition of a prolapsed uterus creates severe disruptions to both everyday activities and sexual relations and general life satisfaction. Most cases of uterine prolapse become manageable through proper Uterine Prolapse Treatment In Bangalore which help women restore their comfort levels and self-confidence.
Symptoms and Causes
Common Symptoms
- Pelvic Pressure or Fullness: A sensation of heaviness or pressure in the pelvic region.
- More Advanced Cases: In some more advanced cases, you may see or feel tissue coming out from the vagina.
- Lower Back Ache: Discomfort that may worsen throughout the day or during strenuous activities.
- Urinary Problems: Frequent urination, difficulty starting urine flow, or a feeling that the bladder is not fully emptying are urinary problems.
- Pain or Pressure During Intercourse: Pain or pressure during sexual activity can be a sign of a prolapse.
Primary Causes
- Pregnancy and Childbirth: Multiple or complicated vaginal births can weaken or tear pelvic floor muscles and ligaments.
- Weakened pelvic support structures: This is due to decreased estrogen levels, especially after menopause.
- Excess weight: Weight puts pressure on the pelvic area, possibly speeding up weakening of the muscles and ligaments.
- Chronic Straining: Persistent coughing, constipation, or heavy lifting can be chronic straining of the pelvic floor.
- Predisposition: Some women have naturally weaker connective tissues that make them more prone to prolapse.
The first step to preventing the condition from worsening is to recognize these symptoms early and understand what causes them. Persistent pelvic discomfort or any sign of prolapse requires professional evaluation.
Diagnosis of Uterine Prolapse
A doctor will usually begin by asking about your medical history and discussing your symptoms to diagnose uterine prolapse. After a pelvic exam, you may be asked to bear down as if you were having a bowel movement. It helps to show the degree of prolapse. Additional tests may be recommended in some cases.
- Pelvic Ultrasound: Offers visual insights into the uterus’s position and the state of nearby organs.
- MRI Scan: Provides a comprehensive image if more detailed information is needed.
- Bladder Function Tests: To assess any associated urinary complications.
These findings are based on the grading of the severity of uterine prolapse on a scale. While mild prolapse may not always need immediate intervention, moderate to severe prolapse often does.
Potential Side Effects of Untreated Uterine Prolapse
Complications can occur if uterine prolapse is left untreated or if treatment is delayed.
Urinary tract infections: Ongoing difficulty in emptying the bladder may increase the risk of urinary tract infections.
- Urinary Issues: Persistent pain and pelvic pressure can make it difficult to complete day-to-day tasks and physical activities.
- Sexual Dysfunction: The further the uterus descends, the more uncomfortable or painful intimacy may be.
- Advanced prolapse: A more advanced prolapse can cause bowel movement problems such as constipation or incomplete evacuation.
- Quality of Life Decline: The physical and emotional burden can lead to a lowering of self confidence and overall quality of life.
Early diagnosis and prompt management are essential to prevent these potential side effects and to allow women to live a comfortable, active life.
Treatment Options
Conservative Methods
- Kegels (Pelvic Floor Exercises): Exercises to strengthen the muscles that support the uterus. As time goes on, mild prolapse symptoms can be reduced by a more robust pelvic floor.
- Pessary: Removable silicone device placed in the vagina to support the uterus (pessary). There are many different shapes and sizes of pessaries and they can be a very effective and non-surgical option for those with moderate prolapse or those who wish to avoid or delay surgery.
Medical and Surgical Interventions
- Topical Estrogen Creams or Rings: Hormone therapy can be used to restore pelvic tissue strength in peri or post menopausal women.
- Surgical Repair: There are several different surgeries that attempt to put the uterus back into place or remove it if that is necessary. In severe cases, procedures may include repairing pelvic floor muscles, tightening ligaments or performing a hysterectomy.
- Specific situations: Doctors may use synthetic mesh to fortify the pelvic floor in certain situations. Mesh procedures are however considered carefully on the basis of individual needs and risks.
It is important to discuss your specific symptoms, lifestyle and future plans with your healthcare provider before making any decision. Personalized treatment leads to the best outcomes and a faster return to daily activities.
Dr. Archana Agarwal’s Approach
Dr. Archana Agarwal is a gynecologist and fertility specialist who is dedicated to the patient first and takes a uterine prolapse patient-first approach. First, she listens to each patient’s concerns, then carefully evaluates the patient to accurately determine the stage of prolapse. She is committed to keeping up with the latest medical advances and provides safe, evidence-based treatments.
Dr. Archana goes beyond treating physical problems, as she knows the emotional struggles of uterine prolapse. She will take the time to explain every treatment plan in simple terms so that you feel informed and comfortable. Dr. Archana is dedicated to providing personalized care in every step, whether you need help with lifestyle modifications, pessary care or advanced surgical interventions.
Last Words
Your health and comfort matter. If you are experiencing symptoms such as pelvic pressure, urinary difficulties or visible protrusion, it is best to seek a professional assessment sooner rather than later. Uterine prolapse can be treated effectively by conservative methods, advanced treatments, and lifestyle changes. Dr. Archana Agarwal’s expertise and compassionate care will help you restore pelvic stability and regain control over your daily life.
Frequently asked questions
How do I know if I have uterine prolapse?
Symptoms may include a feeling of heaviness in the pelvis, tissue protruding from the vagina, and pelvic pain with physical activities. If you have these symptoms, see a qualified gynecologist for a complete evaluation.
Is uterine prolapse treatable without surgery?
Yes. Pelvic floor exercises or pessary devices sometimes can manage mild to moderate cases. The best way to go about it will depend on the severity of your prolapse and your general health.
Does uterine prolapse affect fertility?
In some cases it can complicate pregnancy. If you are planning to conceive, talk to a specialist about safe and effective ways to manage your pregnancy before conception.
What lifestyle changes can help prevent worsening prolapse?
To prevent further weakening of supportive tissues, maintain a healthy weight, perform regular pelvic floor exercises, and avoid heavy lifting or chronic straining.
Are there risks associated with surgical repair?
There are potential risks as with any surgery such as infection, bleeding or anesthesia complications. Your doctor will discuss all possible risks and benefits of the treatment based on your particular condition.
What is a pessary, and how often should it be replaced?
There is a silicone device called a pessary that is placed in the vagina to support the uterus. It should be cleaned regularly and the replacement or adjustment varies from patient to patient and the type of device.
Can uterine prolapse reoccur after treatment?
Treatment is directed at correcting or managing prolapse, but recurrence is common, particularly if there is no follow-up care and no continuation of pelvic floor exercises. It allows you to track any changes.
How long does recovery take after surgical treatment?
The type of surgery and individual healing rates will determine how long it takes to recover, from a few weeks to a few months. Your doctor will give you personalized guidelines to help you recover smoothly.
Is it safe to have sexual intercourse with uterine prolapse?
Prolapse may not affect sexual activity if mild, but moderate to severe prolapse can lead to discomfort. If you’re in pain, talk to your doctor about safe and comfortable options for intimacy.
When should I seek medical help for possible uterine prolapse?
If you have persistent pelvic pressure, difficulty urinating, or tissue bulging from the vagina, it is a good idea to see a medical professional as soon as possible for a correct diagnosis and timely treatment. Control of your pelvic health is a step to long-term well-being. If you have a suspicion that you have uterine prolapse or want to know more, then you can contact a qualified professional such as Dr. Archana Agarwal, a gynecologist, to guide you in the right direction. Keeping yourself informed and proactive will help you overcome uterine prolapse and live a healthier, more confident life.

 +91 93807 91398
+91 93807 91398